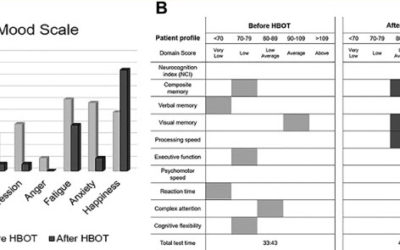
Returning veterans are frequently diagnosed with traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). Considering a recent case-controlled study of hyperbaric oxygen therapy (HBOT) reporting a reduction in suicidal ideation, we investigated retrospectively three veterans with chronic TBI/PTSD symptoms who were treated with multiple rounds of HBOT with neurophysiological testing performed before and after treatment. Improvements were detected on parameters within neurocognitive domains, including reductions in suicide-related symptoms. These findings independently confirm that HBOT may be effective in treating specific symptoms of TBI/PTSD that are not currently addressed with existing therapeutic approaches.
Evidence brief: hyperbaric oxygen therapy (HBOT) for traumatic brain injury and/or post-traumatic stress disorder.
This report is a product of the VA Evidence-based Synthesis Program. The purpose is to provide “timely and accurate syntheses of targeted healthcare topics. to improve the health and healthcare of Veterans”. The authors have made a comprehensive search and analysis of the literature and make recommendations to assist clinicians in dealing with veterans suffering from either traumatic brain injury (TBI) or post-traumatic stress disorder (PTSD). The report is timely and of great potential impact given the vigorous and lengthy debate among hyperbaric physicians and lay people determined to find an answer for the large numbers of veterans deeply affected with some combination of PTSD and post-concussion dysfunction.
HYPERBARIC OXYGEN THERAPY- BASICS AND NEW APPLICATIONS
Hyperbaric oxygen therapy (HBOT) serves as primary or adjunctive therapy for a diverse range of medical conditions. The indication for HBOT can be related to either pressure (decompression sickness or air emboli) or tissue hypoxia. It is now realized, that the combined action of hyperoxia and hyperbaric pressure, leads to significant improvement in tissue oxygenation while targeting both oxygen and pressure sensitive genes, resulting in improved mitochondrial metabolism with anti-apoptotic and anti-inflammatory effects. Clinical studies published in recent year’s present convincing evidence that HBOT can be the coveted neurotherapeutic method for brain repair. Here we discuss the multi-faceted role of HBOT in wound care in general and in neurotherapeutics in detail.
Case control study: hyperbaric oxygen treatment of mild traumatic brain injury persistent post-concussion syndrome and post-traumatic stress disorder.
Mild traumatic brain injury (TBI) persistent post-concussion syndrome (PPCS) and post-traumatic stress disorder (PTSD) are epidemic in United States Iraq and Afghanistan War veterans. Treatment of the combined diagnoses is limited. The aim of this study is to assess safety, feasibility, and effectiveness of hyperbaric oxygen treatments (HBOT) for mild TBI PPCS and PTSD. Thirty military subjects aged 18-65 with PPCS with or without PTSD and from one or more blast-induced mild-moderate traumatic brain injuries that were a minimum of 1 year old and occurred after 9/11/2001 were studied. The measures included symptom lists, physical exam, neuropsychological and psychological testing on 29 subjects (1 dropout) and SPECT brain imaging pre and post HBOT.
Hyperbaric oxygen therapy restored traumatic stress-induced dysregulation of fear memory and related neurochemical abnormalities.
Abstract: Individuals with post-traumatic stress disorder (PTSD) are characterized by fear memory problems and hypocortisolemia of which traumatic stress-induced monoaminergic disruption over infralimbic (IL) cortex is considered the key mechanism. Hyperbaric oxygen...
Hyperbaric oxygen therapy restored traumatic stress-induced dysregulation of fear memory and related neurochemical abnormalities.
Individuals with posttraumatic stress disorder (PTSD) are characterized by fear memory problems and hypocortisolemia of which traumatic stress-induced monoaminergic disruption over infralimbic (IL) cortex is considered the key mechanism. Hyperbaric oxygen therapy (HBOT) has recently proven its utility in treating several mental disorders but remains unexplored for PTSD. The present study aimed to examine the effects of 5-day HBO paradigm on traumatic stress (single prolonged stress, SPS, an animal model of PTSD)-induced dysregulation of fear memory/anxiety profiles and related abnormalities in IL monoamines and plasma corticosterone.
Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy.
Traumatic brain injury (TBI) may cause persistent cognitive dysfunction. A pilot clinical study was performed to determine if hyperbaric oxygen (HBO₂) treatment improves cognitive performance. It was hypothesized that stem cells, mobilized by HBO₂ treatment, are recruited to repair damaged neuronal tissue. This hypothesis was tested by measuring the relative abundance of stem cells in peripheral blood and cognitive performance during this clinical trial. The subject population consisted of 28 subjects with persistent cognitive impairment caused by mild to moderate TBI suffered during military deployment to Iraq or Afghanistan. Fluorescence-activated cell sorting (FACS) analysis was performed for stem cell markers in peripheral blood and correlated with variables resulting from standard tests of cognitive performance and post-traumatic stress disorder: ImPACT, BrainCheckers and PCL-M test results. HBO₂ treatment correlated with stem cell mobilization as well as increased cognitive performance. Together these results support the hypothesis that stem cell mobilization may be required for cognitive improvement in this population.
Baseline neurological evaluations in a hyperbaric trial of post-concussive syndrome.
Abstract: Standard neurologic examinations may not detect abnormalities in U.S. military service members with persistent post-concussive symptoms following mild traumatic brain injury. The Brain Injury and Mechanisms of Action of Hyperbaric Oxygen for Persistent...
Neuropsychological assessments in a hyperbaric trial of post-concussive symptoms.
Results of studies addressing the effect of mild traumatic brain injury (mTBI) and post-traumatic stress disorder (PTSD) on symptoms and neuropsychological assessments are mixed regarding cognitive deficits in these populations. Neuropsychological assessments were compared between U.S. military service members with mTBI only (n=36) vs. those with mTBI÷ PTSD (n=35) from a randomized interventional study of mTBI participants with persistent post-concussive symptoms (PCS). The mTBI group endorsed worse symptoms than published norms on PCS, PTSD and pain scales (⟩50% abnormal on Neurobehavioral Symptom Inventory (NSI), PTSD Checklist-Civilian, McGill Pain Questionnaire-Short Form) and some quality of life domains.
Sleep assessments for a mild traumatic brain injury trial in a military population.
Abstract: Baseline sleep characteristics were explored for 71 U.S. military service members with mild traumatic brain injury (mTBI) enrolled in a post-concussive syndrome clinical trial. The Pittsburgh Sleep Quality Index (PSQI), sleep diary, several disorder-specific...